Medicaid is the public health insurance program for low-income Americans. Medicaid, combined with the Children’s Health Insurance Program (CHIP), covers 72,918,167 individuals — 66,346,562 are covered by Medicaid and 6,571,605 in CHIP. The Medicaid and CHIP data book estimates that 29.1 percent of the population was enrolled in Medicaid or CHIP at some point in 2017.
The program is a collaboration between the federal government and individual states, with each paying a share of the cost. The percentage of the cost paid by the federal government varies by state but averaged 61.5 percent in 2017. Montana had the highest percentage paid by the federal government at 80 percent, and New York had the lowest at 48.8 percent.
Similar to Medicare, the program uses a combination of public and private insurance programs. Over two-thirds of Medicaid enrollees are in a private managed care program. States choose whether to contract with private insurance companies or whether to use a public fee for service benefit and provider payment system.
ACA and Medicaid
The Affordable Care Act (ACA) attempted to reduce the number of uninsured Americans by expanding Medicaid eligibility. Medicaid eligibility and benefits varied by state prior to the ACA. The law mandated that states expand eligibility to a common standard and provide consistent benefit levels. The federal government paid 100 percent of the cost of the newly eligible individuals for the first few years, with a declining schedule to 90 percent by 2020 and beyond. The Supreme Court deemed the action by the federal government through the ACA to be unconstitutional coercion. The Court determined that the federal government could not force this expense on states. The remedy for the unconstitutionality was to give states the choice of whether or not to expand Medicaid eligibility to the federal standard.
The Supreme Court’s remedy decision resulted in state choice regarding Medicaid eligibility expansion. As of this writing, 14 states had chosen to not comply with the ACA expansion. These include:
- Alabama
- Florida
- Georgia
- Kansas
- Mississippi
- Missouri
- North Carolina
- Oklahoma
- South Carolina
- South Dakota
- Tennessee
- Texas
- Wisconsin
- Wyoming
If the federal government is covering 90 percent of the ongoing cost for newly eligible individuals, why wouldn’t a state expand eligibility? It could simply be revenge politics with Republican governors resisting the Democrat-authored expansion. It could also be fear of a false promise. Although the ACA requires that the federal government will pay 90 percent of the cost for newly eligible individuals, there is no permanent guarantee from the federal government. In fact, the Congressional Budget Office (CBO) financially scored the concept of limiting the federal government’s funding for Medicaid in November 2013 — before the January 1, 2014, expansion even started. Whether Congress ever intends to reduce the federal government’s commitment to funding Medicaid expansion is not known, but the CBO continues to provide financial estimates for shifting financial responsibility to states by capping the federal government’s spending on Medicaid.
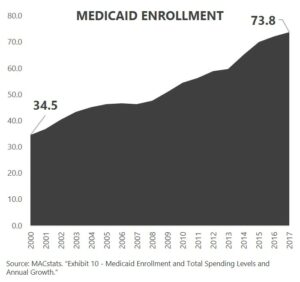
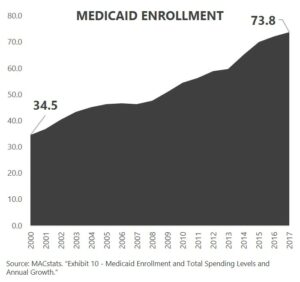
Medicaid Enrollment
The number of individuals covered by Medicaid and CHIP has grown significantly, even with some states electing to not expand eligibility. Enrollment has more than doubled since 2000.
What’s Next?
The 14 states that have not expanded eligibility will continue to face pressure to do so. Leaving the economically neediest in society without health insurance coverage is a social justice question and challenge that will not go away.
The federal government is already signaling that it may need to find ways to contain its Medicaid spending. The options for which the CBO has produced financial estimates provide an indication of potential future direction — putting significant financial pressure on states.
States will continue to find innovative ways to contain Medicaid pricing. Medicaid is delivered on a state-specific delivery platform. Each state effectively has its own network or provider reimbursement strategy. Expect significant state pressure to control spending as inflation and enrollment continue to grow.
Next week, I’ll take a look at employer-sponsored health insurance and what this means with the election approaching. Be sure to tune in. And, if you haven’t already, I encourage you to sign up for our “Insiders’ Club” where you’ll be notified when I release new information AND receive a FREE copy of my book “The Voter’s Guide to Healthcare: A non-partisan, candid, and relevant look at politics and healthcare in America” when it’s available.